Rural healthcare has long faced challenges due to limited resources, geographic location, and difficulty recruiting and retaining qualified healthcare professionals. To make matters worse, after the height of the pandemic, many rural healthcare practices were forced to close their doors, leaving an already vulnerable patient population with a lack of accessible healthcare.
Barriers to Care for Rural Communities
Residents of rural communities often face a variety of barriers to healthcare that include limited access to specialized care, lack of transportation, higher rates of chronic diseases, and limited internet access. These disparities can lead to poor health outcomes and increased care costs. Individuals living in rural areas are also more likely to die from heart disease, cancer, unintentional injury, chronic lower respiratory disease, and stroke than their urban counterparts.
Addressing health disparities in rural communities requires a multifaceted approach that includes leveraging technology such as telehealth and remote patient monitoring. Through the 2024 Final Medicare Physician Fee Schedule released November 2, 2023, Rural Health Centers (RHCs) and Federally Qualified Health Centers (FQHCs) will now be able to receive Medicare reimbursement for telehealth and remote patient monitoring services, which is a long-awaited step in the right direction for expanding access to care for rural patients.
How Remote Care Can Help Reduce Barriers to Care for Rural Health Communities
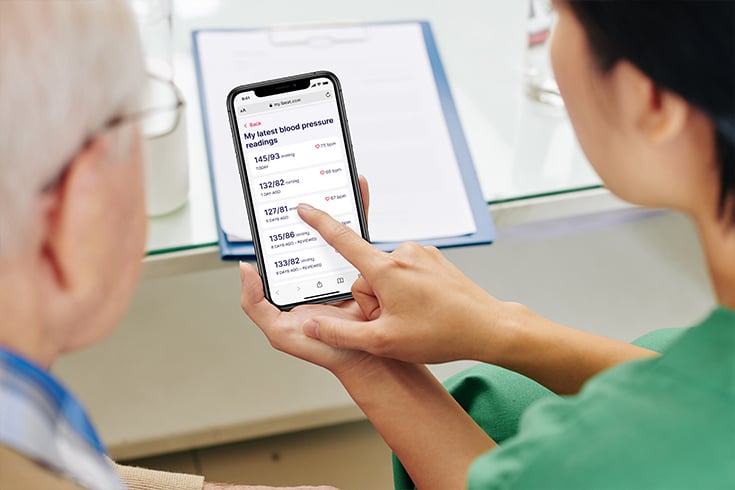
By enabling rural healthcare providers to monitor and manage patients’ health remotely, RHCs and FQHCs can deliver greater access to effective, personalized care. In fact, many rural healthcare facilities have already seen success through implementing remote patient monitoring programs.
For example, one provider using the 100Plus’ AI-enabled remote patient monitoring (RPM) solution recounts his experience with remote monitoring in a rural practice. He said it “fosters a collaboration that reduces the feelings of isolation that physicians may experience when they go to practice in a small town.” He described remote care as “having one foot in the city but being able to live and practice out in a rural area” and found it “reassuring to know that you’re on the right track with the treatment plan and are staying current.”
Another example is Greenville Healthcare Associates, a midsized family practice that services hundreds of rural patients in North Texas. The implementation of remote patient monitoring was especially beneficial to their rural patients with chronic conditions, many of whom needed to travel long distances to come into their office for their regular screenings. The practice’s program manager, Nadia Ziyadeh-Hammad, shared, “We have seen tremendous results from patients enrolled with the 100Plus RPM. Their clinical health metrics improved, they have become more engaged in their health, and more compliant with their care plans.”
AI-enabled RPM enables clinicians to remotely monitor and manage the health of their patients from the comfort of their homes, which can be especially beneficial to rural patients. Providers can detect deteriorating conditions earlier, leading to more timely interventions and better health outcomes.
Benefits of AI-enabled RPM in Rural Health Communities
AI-enabled RPM can help address many of the challenges faced by rural health communities, including:
Reducing Travel Burden
AI-enabled RPM can bridge geographic barriers by enabling clinicians to manage a patient’s care outside brick-and-mortar care settings, often reducing the need for regular physical visits. This is a significant advantage for rural patients, especially those with limited access to transportation.
Improving Adherence
Certain remote care programs can remind patients to take their vitals and medications. This helps with better disease management and prevents complications. One example of this is with AI virtual health assistants like Esper. This intelligent technology is designed to provide a more personalized, convenient, and proactive care experience that delivers patient outreach on behalf of medical practices through phone and SMS text communications.
AI virtual health assistants can offer 24/7 support, answer questions, deliver health information, and provide alert reminders to ensure patients adhere to their care plans. In addition, AI virtual assistants can help reduce some of the administrative burden for healthcare staff, enabling them to concentrate more of their efforts on patient care.
Lowering Costs and Increasing Reimbursement
Through earlier interventions and better disease management, remote patient monitoring can help reduce hospital admissions and emergency room visits, which results in significant cost savings for both patients and healthcare facilities. It can also help boost reimbursement for rural clinics while enabling expanded access to care for their patients. Additionally, certain RPM programs provide ready-to-use devices with integrated cellular connectivity that does not require internet, so patients without broadband access are able to bypass these barriers.
Not only does AI-enabled RPM enable clinicians to remotely monitor and manage the health of their patients from the comfort of their homes, but it also helps rural communities overcome many barriers to care. Whether implemented for diabetes management, COPD, hypertension, CHF, or maternal care, AI-enabled RPM is a powerful tool that can benefit rural communities by making care more accessible and effective. What’s more, now that FQHCs and RHCs can receive reimbursement for providing these vital services, more patients will get access to the care they so desperately need.
Start The Path Toward Better Patient Care
Have questions about how remote patient monitoring for healthcare will work for you and your patients? Let’s have a conversation.
Access the Latest RPM News
Stay up to date with the latest news, articles and webinars about remote patient monitoring and telehealth.
"*" indicates required fields