Though many patients recover from COVID-19 within a few weeks, some experience new, recurring, or ongoing symptoms four or more weeks after infection. According to a recent analysis of records from nearly two million patients, long COVID, also referred to as post-acute COVID-19, chronic COVID, long-haul COVID, late sequelae and others, may affect nearly 25% of persons infected with SARS-CoV-2, presenting a significant medical management challenge for healthcare providers.
As more cases of long COVID come to light and infectious variants continue to increase the risk of viral spread, remote patient monitoring could be a useful resource in tracking symptoms and related health information in order to better understand and treat long COVID, especially in chronically ill patients in the Medicare population.
The threat of long COVID conditions
Currently, long COVID conditions represent a wide range of health consequences and symptoms that present four or more weeks after initial infection of SARS-CoV-2. Though researchers are still investigating prevalence, mechanism, duration, and severity of conditions and symptoms associated with long COVID, here are some of the most common long COVID conditions reported by the CDC:
- Multiorgan System Effects: Affecting cardiovascular, pulmonary, renal, dermatologic, neurologic, and psychiatric body systems. Multisystem inflammatory syndrome (MIS) and autoimmune conditions can also arise.
- Effects of COVID-19 Illness or Hospitalization: Severe illness and hospitalization due to COVID-19 can result in effects similar to those from hospitalization for other respiratory infections or conditions, including tracheal stenosis, severe weakness, and deconditioning. Additional impact of severe illness or hospitalization can include:
- Post-intensive care syndrome (PICS)
- Post-traumatic stress disorder (PTSD)
- New or Ongoing Symptoms: Patients who have had mild, asymptomatic, or severe COVID-19 can experience a diverse range of new or persistent symptoms, including:
- Dyspnea or increased respiratory effort
- Fatigue
- Cough
- Chest pain
- Headache
- Palpitations and/or tachycardia
- Arthralgia
- Myalgia
- Abdominal pain
- Diarrhea
- Insomnia
- Fever
- Impaired daily function and mobility
It’s important to note that these categories do not exist independently from one another: patients can experience an overlap of multiorgan complications, effects of treatment or hospitalization, and new or ongoing symptoms.
The unique challenges of evaluating and caring for patients with long COVID
The goal of medical management of long COVID is to optimize function and quality of life. While the rise in virtual care during the pandemic has enabled patients to get basic care during periods of physical inaccessibility, virtual visits on their own cannot provide the level of monitoring and data-collection needed to support long COVID patients in the long term.
What’s more, people with disabilities or chronic health conditions unrelated to COVID-19 may require more monitored and consistent care. The CDC recommends a post-COVID management plan that includes symptom monitoring, patient diaries and reporting, and regular consultations with a healthcare professional in frequency based on the patient’s overall health and illness progression.
Finally, many long-term COVID-19 effects are still unknown. As evidence of its effects continue to emerge, researchers are urging providers to closely monitor patients who have recovered from COVID-19 to see how their organs and body systems are functioning.
Monitoring long COVID and improving patient outcomes with remote patient monitoring
Before COVID-19, remote patient monitoring (RPM) emerged as a critical method to address a growing need to serve seniors and the chronically ill at home, providing an accessible and effective method of managing health and improving outcomes. Since the pandemic, RPM continues to provide necessary care to at-risk populations.
Specifically, RPM is coming to the forefront as an invaluable tool for monitoring patients with suspected or confirmed long COVID, especially if those individuals are unable to access a larger health care facility, whether due to disability, access, or health risk.
What is remote patient monitoring?
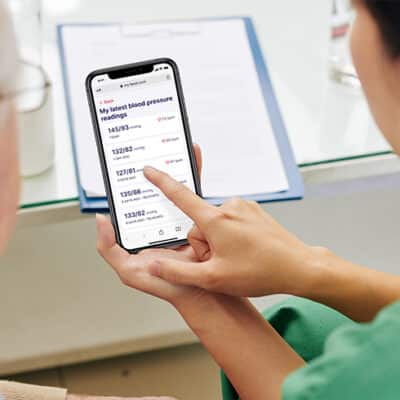
RPM enables healthcare providers to monitor patients’ health outside of physical clinic locations. RPM allows physicians to view continuous patient health data and improve patient outcomes by preemptively managing patient care before episodic care events occur.
Patient perspectives on RPM for COVID-19 care
Managing stress and other mental health disorders associated with acute or long COVID infection is a critical component of COVID care strategy. Between August 2020 and February 2021 alone, the CDC reported the percentage of adults with recent symptoms of an anxiety or a depressive disorder increased from 36.4% to 41.5%. The significant increase in symptoms of mental health disorders is attributed in large part to the grief and fear associated with the pandemic.
In addition to improving facilitation and monitoring of patient symptoms, RPM can also improve patient perception of care and reduce care-related anxiety.
In a survey of nearly 500 remotely-monitored oncology patients, 85% of respondents reported that “RPM was worthwhile, enabled better management of their COVID-19 symptoms, made them feel more connected to their healthcare team, and helped prevent emergency room visits.”
At Blessing Health System in Quincy, Illinois, RPM as part of a larger telehealth action plan enabled providers to minimize patient anxiety while still offering a human-centered and safe recovery plan.
How 100Plus can help facilitate your long COVID patient management and care plan
With 100Plus’ RPM platform, physicians can provide health monitoring devices such as a blood pressure monitor, blood glucose meter, digital scale, and pulse oximeter. We are also the only RPM solution to utilize AI and offer an end-to-end solution, including patient outreach, device setup, and patient engagement and education.
With the help of Esper, our AI-enabled, text message based chatbot, your practice can:
- Scale your RPM program faster
- Better onboard and educate patients
- Gather more readings for better calibration of patient care plans in-between visits
- Answer your patients’ miscellaneous questions, reducing call and email output
RPM is effective at monitoring at-risk patients with long COVID
Though researchers are still learning about the scale, prevalence, and duration of long COVID, evidence shows that RPM can provide effective and easy-to-use tools for monitoring at-home and at-risk patients.